Stoners coming out – beyond the marijuana monster myths | David Schmader | TEDxRainier
In this funny, informative talk, David Schmader makes the case for thinking more broadly about what a marijuana user is and can be.
Cannabis (drug)
Cannabis, also known as marijuana among other names,[a] is a psychoactive drug from the Cannabis plant. Native to Central Asia and the Indian subcontinent, the cannabis plant has been used as a drug for both recreational and entheogenic purposes and in various traditional medicines for centuries.[18][19][20] Tetrahydrocannabinol (THC) is the main psychoactive component of cannabis, which is one of the 483 known compounds in the plant,[21] including at least 65 other cannabinoids,[22] including cannabidiol (CBD).[23] Cannabis can be used by smoking, vaporizing, within food, or as an extract.[24]
Cannabis has various mental and physical effects, which include euphoria, altered states of mind and sense of time, difficulty concentrating, impaired short-term memory and body movement,[24] relaxation,[25] and an increase in appetite.[26] Onset of effects is felt within minutes when smoked, and about 30 to 60 minutes when cooked and eaten.[24][27] The effects last for two to six hours, depending on the amount used.[27] At high doses, mental effects can include anxiety, delusions (including ideas of reference), hallucinations, panic, paranoia, and psychosis.[24][23] There is a strong relation between cannabis use and the risk of psychosis,[28][29] though the direction of causality is debated.[30] Physical effects include increased heart rate, difficulty breathing, nausea, and behavioral problems in children whose mothers used cannabis during pregnancy;[24] short-term side effects may also include dry mouth and red eyes.[31][32] Long-term adverse effects may include addiction, decreased mental ability in those who started regular use as adolescents, chronic coughing, susceptibility to respiratory infections,[33] and cannabinoid hyperemesis syndrome.
Cannabis is mostly used recreationally or as a medicinal drug, although it may also be used for spiritual purposes. In 2013, between 128 and 232 million people used cannabis (2.7% to 4.9% of the global population between the ages of 15 and 65).[34] It is the most commonly used illegal drug in the world,[24][34] though it is legal in some jurisdictions, with the highest use among adults (as of 2018) in Zambia, the United States, Canada, and Nigeria.[35]
While cannabis plants have been grown since at least the 3rd millennium BCE,[36] evidence suggests that it was being smoked for psychoactive effects at least 2,500 years ago in the Pamir Mountains;[37] the earliest evidence found at a cemetery in what is today western China close to the tripoint with Tajikistan and Afghanistan.[38] Since the early 20th century, cannabis has been subject to legal restrictions. The possession, use, and cultivation of cannabis is illegal in most countries of the world.[39][40] In 2013, Uruguay became the first country to legalize recreational use of cannabis.[41] Other countries to do so are Canada, Georgia, and South Africa, plus 18 states, two territories, and the District of Columbia in the United States (though the drug remains federally illegal).[41][42] Medical use of cannabis, requiring the approval of a physician, has been legalized in a greater number of countries.[43]
Uses
Medical
Medical cannabis, or medical marijuana, can refer to the use of cannabis and its cannabinoids to treat disease or improve symptoms; however, there is no single agreed-upon definition.[44][45] The rigorous scientific study of cannabis as a medicine has been hampered by production restrictions and by the fact that it is classified as an illegal drug by many governments.[46] There is limited evidence suggesting cannabis can be used to reduce nausea and vomiting during chemotherapy, to improve appetite in people with HIV/AIDS, or to treat chronic pain and muscle spasms.[47][48][49] Its use for other medical applications is insufficient for drawing conclusions about safety or efficacy.
Short-term use increases the risk of both minor and major adverse effects.[48] Common side effects include dizziness, feeling tired and vomiting.[48] The long-term effects of cannabis are not clear.[48] There are concerns surrounding memory and cognition problems, risk of addiction, risk of schizophrenia in young people, and the risk of children taking it by accident.[47]
Recreational
Cannabis has psychoactive and physiological effects when consumed.[50] The immediate desired effects from consuming cannabis include relaxation and euphoria (the “high” or “stoned” feeling), a general alteration of conscious perception, increased awareness of sensation, increased libido[25] and distortions in the perception of time and space. At higher doses, effects can include altered body image, auditory and/or visual illusions, pseudohallucinations and ataxia from selective impairment of polysynaptic reflexes.[citation needed] In some cases, cannabis can lead to dissociative states such as depersonalization[51][52] and derealization.[53]
Some immediate undesired side effects include a decrease in short-term memory, dry mouth, impaired motor skills and reddening of the eyes.[54] Aside from a subjective change in perception and mood, the most common short-term physical and neurological effects include increased heart rate, increased appetite and consumption of food, lowered blood pressure, impairment of short-term and working memory,[55][56] psychomotor coordination, and concentration. Some users may experience an episode of acute psychosis, which usually abates after six hours, but in rare instances, heavy users may find the symptoms continuing for many days.[57]
A reduced quality of life is associated with heavy cannabis use, although the relationship is inconsistent and weaker than for tobacco and other substances.[58] The direction of cause and effect, however, is unclear.[58]
Spiritual
Cannabis has held sacred status in several religions and has served as an entheogen – a chemical substance used in religious, shamanic, or spiritual contexts[59] – in the Indian subcontinent since the Vedic period dating back to approximately 1500 BCE, but perhaps as far back as 2000 BCE. There are several references in Greek mythology to a powerful drug that eliminated anguish and sorrow. Herodotus wrote about early ceremonial practices by the Scythians, thought to have occurred from the 5th to 2nd century BCE. In modern culture, the spiritual use of cannabis has been spread by the disciples of the Rastafari movement who use cannabis as a sacrament and as an aid to meditation. The earliest known reports regarding the sacred status of cannabis in the Indian subcontinent come from the Atharva Veda, estimated to have been composed sometime around 1400 BCE.[60]
Available forms
Cannabis is consumed in many different ways,[61] all of which involve heating to decarboxylate THCA in the plant into THC.[62]
- Smoking, which typically involves burning and inhaling vaporized cannabinoids (“smoke”) from small pipes, bongs (portable versions of hookahs with a water chamber), paper-wrapped joints or tobacco-leaf-wrapped blunts, and other items.[63]
- Vaporizer, which heats any form of cannabis to 165–190 °C (329–374 °F),[64] causing the active ingredients to evaporate into vapor without burning the plant material (the boiling point of THC is 157 °C (315 °F) at atmospheric pressure).[65]
- Cannabis tea, which contains relatively small concentrations of THC because THC is an oil (lipophilic) and is only slightly water-soluble (with a solubility of 2.8 mg per liter).[66] Cannabis tea is made by first adding a saturated fat to hot water (e.g. cream or any milk except skim) with a small amount of cannabis.[67]
- Edibles, where cannabis is added as an ingredient to one of a variety of foods, including butter and baked goods. In India it is commonly made into a beverage, bhang.
- Capsules, typically containing cannabis oil, and other dietary supplement products, for which some 220 were approved in Canada in 2018.[68]
Adverse effects

Short term
Acute effects may include anxiety and panic, impaired attention and memory, an increased risk of psychotic symptoms,[b] the inability to think clearly, and an increased risk of accidents.[72][73][23] Cannabis impairs a person’s driving ability, and THC was the illicit drug most frequently found in the blood of drivers who have been involved in vehicle crashes. Those with THC in their system are from three to seven times more likely to be the cause of the accident than those who had not used either cannabis or alcohol, although its role is not necessarily causal because THC stays in the bloodstream for days to weeks after intoxication.[74][75][c]
According to the United States Department of Health and Human Services, there were 455,000 emergency room visits associated with cannabis use in 2011. These statistics include visits in which the patient was treated for a condition induced by or related to recent cannabis use. The drug use must be “implicated” in the emergency department visit, but does not need to be the direct cause of the visit. Most of the illicit drug emergency room visits involved multiple drugs.[78] In 129,000 cases, cannabis was the only implicated drug.[79][80]
The short term effects of cannabis can be altered if it has been laced with opioid drugs such as heroin or fentanyl.[81] The added drugs are meant to enhance the psychoactive properties, add to its weight, and increase profitability, despite the increased danger of overdose.[82][83][d]
Long term
Heavy, long-term exposure to marijuana may have biologically-based physical, mental, behavioral and social health consequences. It may be “associated with diseases of the liver (particularly with co-existing hepatitis C), lungs, heart, and vasculature”.[85] Mothers who used marijuana during pregnancy have children with elevated levels of depression, hyperactivity, impulsivity and inattention.[86] It is recommended that cannabis use be stopped before and during pregnancy as it can result in negative outcomes for both the mother and baby.[87][88] However, maternal use of marijuana during pregnancy does not appear to be associated with low birth weight or early delivery after controlling for tobacco use and other confounding factors.[89] A 2014 review found that while cannabis use may be less harmful than alcohol use, the recommendation to substitute it for problematic drinking was premature without further study.[90] Various surveys conducted between 2015 and 2019 found that many users of cannabis substitute it for prescription drugs (including opioids), alcohol, and tobacco; most of those who used it in place of alcohol or tobacco either reduced or stopped their intake of the latter substances.[91]
A limited number of studies have examined the effects of cannabis smoking on the respiratory system.[92] Chronic heavy marijuana smoking is associated with coughing, production of sputum, wheezing, and other symptoms of chronic bronchitis.[72] The available evidence does not support a causal relationship between cannabis use and chronic obstructive pulmonary disease.[93] Short-term use of cannabis is associated with bronchodilation.[94] Other side effects of cannabis use include cannabinoid hyperemesis syndrome (CHS), a condition which involves recurrent nausea, cramping abdominal pain, and vomiting.[95]
Cannabis smoke contains thousands of organic and inorganic chemical compounds. This tar is chemically similar to that found in tobacco smoke,[96] and over fifty known carcinogens have been identified in cannabis smoke,[97] including; nitrosamines, reactive aldehydes, and polycylic hydrocarbons, including benz[a]pyrene.[98] Cannabis smoke is also inhaled more deeply than tobacco smoke.[99] As of 2015, there is no consensus regarding whether cannabis smoking is associated with an increased risk of cancer.[100] Light and moderate use of cannabis is not believed to increase risk of lung or upper airway cancer. Evidence for causing these cancers is mixed concerning heavy, long-term use. In general there are far lower risks of pulmonary complications for regular cannabis smokers when compared with those of tobacco.[101] A 2015 review found an association between cannabis use and the development of testicular germ cell tumors (TGCTs), particularly non-seminoma TGCTs.[102] Another 2015 meta-analysis found no association between lifetime cannabis use and risk of head or neck cancer.[103] Combustion products are not present when using a vaporizer, consuming THC in pill form, or consuming cannabis foods.[104]
There is concern that cannabis may contribute to cardiovascular disease,[105] but as of 2018, evidence of this relationship was unclear.[106] Research in these events is complicated because cannabis is often used in conjunction with tobacco, and drugs such as alcohol and cocaine that are known to have cardiovascular risk factors.[107] Smoking cannabis has also been shown to increase the risk of myocardial infarction by 4.8 times for the 60 minutes after consumption.[108]
Neuroimaging
Although global abnormalities in white matter and grey matter are not associated with heavy cannabis use, reduced hippocampal volume is consistently found.[109] Amygdala abnormalities are sometimes reported, although findings are inconsistent.[110][111][112]
Cannabis use is associated with increased recruitment of task-related areas, such as the dorsolateral prefrontal cortex, which is thought to reflect compensatory activity due to reduced processing efficiency.[112][111][113] Cannabis use is also associated with downregulation of CB1 receptors. The magnitude of down regulation is associated with cumulative cannabis exposure, and is reversed after one month of abstinence.[114][115][116] There is limited evidence that chronic cannabis use can reduce levels of glutamate metabolites in the human brain.[117]
Cognition
A 2015 meta-analysis found that, although a longer period of abstinence was associated with smaller magnitudes of impairment, both retrospective and prospective memory were impaired in cannabis users. The authors concluded that some, but not all, of the deficits associated with cannabis use were reversible.[118] A 2012 meta-analysis found that deficits in most domains of cognition persisted beyond the acute period of intoxication, but was not evident in studies where subjects were abstinent for more than 25 days.[119] Few high quality studies have been performed on the long-term effects of cannabis on cognition, and the results were generally inconsistent.[120] Furthermore, effect sizes of significant findings were generally small.[119] One review concluded that, although most cognitive faculties were unimpaired by cannabis use, residual deficits occurred in executive functions.[121] Impairments in executive functioning are most consistently found in older populations, which may reflect heavier cannabis exposure, or developmental effects associated with adolescent cannabis use.[122] One review found three prospective cohort studies that examined the relationship between self reported cannabis use and intelligence quotient (IQ). The study following the largest number of heavy cannabis users reported that IQ declined between ages 7–13 and age 38. Poorer school performance and increased incidence of leaving school early were both associated with cannabis use, although a causal relationship was not established.[114] Cannabis users demonstrated increased activity in task-related brain regions, consistent with reduced processing efficiency.[123]
Psychiatric
At an epidemiological level, a dose–response relationship exists between cannabis use and increased risk of psychosis[28][124][125][126] and earlier onset of psychosis.[127] Although the epidemiological association is robust, evidence to prove a causal relationship is lacking.[128] But a biological causal pathway is plausible, especially if there is a genetic predisposition to mental illness, in which case cannabis may be a trigger.[129][better source needed]
It is not clear whether cannabis use affects the rate of suicide.[130][131] Cannabis may also increase the risk of depression, but insufficient research has been performed to draw a conclusion.[132][125] Cannabis use is associated with increased risk of anxiety disorders, although causality has not been established.[133]
A February 2019 review found that cannabis use during adolescence was associated with an increased risk of developing depression and suicidal behavior later in life, while finding no effect on anxiety.[134]
Reinforcement disorders
About 9% of those who experiment with marijuana eventually become dependent according to DSM-IV (1994) criteria.[80] A 2013 review estimates daily use is associated with a 10–20% rate of dependence.[47] The highest risk of cannabis dependence is found in those with a history of poor academic achievement, deviant behavior in childhood and adolescence, rebelliousness, poor parental relationships, or a parental history of drug and alcohol problems.[135] Of daily users, about 50% experience withdrawal upon cessation of use (i.e. are dependent), characterized by sleep problems, irritability, dysphoria, and craving.[114] Cannabis withdrawal is less severe than withdrawal from alcohol.[136]
According to DSM-V criteria, 9% of those who are exposed to cannabis develop cannabis use disorder, compared to 20% for cocaine, 23% for alcohol and 68% for nicotine. Cannabis use disorder in the DSM-V involves a combination of DSM-IV criteria for cannabis abuse and dependence, plus the addition of craving, without the criterion related to legal troubles.[114]
Overdose
There is a perception that cannabis overdose is rare, because the risks of fatality form acute exposure are low in adults.[130] However, there are over 1.5 million visits to the ER as a result of cannabis consumption per year in the US, and the rates are growing significantly with the increased availability and potency of these products following legalization in different states.[137] Legalization has also increased the rates at which children are exposed to cannabis, particularly from edibles. Children under 10 can have far more severe reactions compared to adults, and there have been case reports of death.[138] Children are also at risk for encephalopathy, hypotension, respiratory depression severe enough to require ventilation, somnolence and coma.[139][140]
Severe complications as a result of cannabis use are also rising among adults. At one Colorado medical center following legalization, approximately one quarter of ER admissions for cannabis were for severe, acute psychiatric effects.[141] An additional third of cases were for gastrointestinal issues including cannabinoid hyperemesis syndrome (CHS), a condition seen in chronic cannabis users where they have repeated bouts of uncontrollable vomiting for 24–48 hours. Multiple deaths have been reported as a result of CHS.[142][143]
Pharmacology
Mechanism of action
The high lipid-solubility of cannabinoids results in their persisting in the body for long periods of time.[144] Even after a single administration of THC, detectable levels of THC can be found in the body for weeks or longer (depending on the amount administered and the sensitivity of the assessment method).[144] Investigators have suggested that this is an important factor in marijuana’s effects, perhaps because cannabinoids may accumulate in the body, particularly in the lipid membranes of neurons.[145]
Researchers confirmed that THC exerts its most prominent effects via its actions on two types of cannabinoid receptors, the CB1 receptor and the CB2 receptor, both of which are G protein-coupled receptors.[146] The CB1 receptor is found primarily in the brain as well as in some peripheral tissues, and the CB2 receptor is found primarily in peripheral tissues, but is also expressed in neuroglial cells.[147] THC appears to alter mood and cognition through its agonist actions on the CB1 receptors, which inhibit a secondary messenger system (adenylate cyclase) in a dose-dependent manner.
Via CB1 receptor activation, THC indirectly increases dopamine release and produces psychotropic effects.[148] CBD also acts as an allosteric modulator of the μ- and δ-opioid receptors.[149] THC also potentiates the effects of the glycine receptors.[150] It is unknown if or how these actions contribute to the effects of cannabis.[151]
Chemistry
Detection in body fluids
THC and its major (inactive) metabolite, THC-COOH, can be measured in blood, urine, hair, oral fluid or sweat using chromatographic techniques as part of a drug use testing program or a forensic investigation of a traffic or other criminal offense.[57] The concentrations obtained from such analyses can often be helpful in distinguishing active use from passive exposure, elapsed time since use, and extent or duration of use. These tests cannot, however, distinguish authorized cannabis smoking for medical purposes from unauthorized recreational smoking.[152] Commercial cannabinoid immunoassays, often employed as the initial screening method when testing physiological specimens for marijuana presence, have different degrees of cross-reactivity with THC and its metabolites.[153] Urine contains predominantly THC-COOH, while hair, oral fluid and sweat contain primarily THC.[57] Blood may contain both substances, with the relative amounts dependent on the recency and extent of usage.[57]
The Duquenois–Levine test is commonly used as a screening test in the field, but it cannot definitively confirm the presence of cannabis, as a large range of substances have been shown to give false positives.[154] Researchers at John Jay College of Criminal Justice reported that dietary zinc supplements can mask the presence of THC and other drugs in urine.[155] However, a 2013 study conducted by researchers at the University of Utah School of Medicine refute the possibility of self-administered zinc producing false-negative urine drug tests.[156]
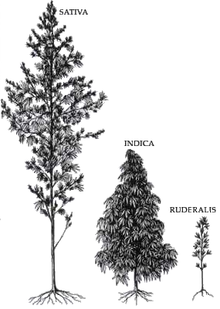
Varieties and strains
CBD is a 5-HT1A receptor agonist, which is under laboratory research to determine if it has an anxiolytic effect.[157] It is often claimed that sativa strains provide a more stimulating psychoactive high while indica strains are more sedating with a body high.[158] However, this is disputed by researchers.[159]
Psychoactive ingredients
According to the United Nations Office on Drugs and Crime (UNODC), “the amount of THC present in a cannabis sample is generally used as a measure of cannabis potency.”[160] The three main forms of cannabis products are the flower/fruit, resin (hashish), and oil (hash oil). The UNODC states that cannabis often contains 5% THC content, resin “can contain up to 20% THC content”, and that “Cannabis oil may contain more than 60% THC content.”[160]
A 2012 review found that the THC content in marijuana had increased worldwide from 1970 to 2009.[161] It is unclear, however, whether the increase in THC content has caused people to consume more THC or if users adjust based on the potency of the cannabis. It is likely that the higher THC content allows people to ingest less tar. At the same time, CBD levels in seized samples have lowered, in part because of the desire to produce higher THC levels and because more illegal growers cultivate indoors using artificial lights. This helps avoid detection but reduces the CBD production of the plant.[162]
Australia’s National Cannabis Prevention and Information Centre (NCPIC) states that the buds (infructescences) of the female cannabis plant contain the highest concentration of THC, followed by the leaves. The stalks and seeds have “much lower THC levels”.[163] The UN states that the leaves can contain ten times less THC than the buds, and the stalks one hundred times less THC.[160]
After revisions to cannabis scheduling in the UK, the government moved cannabis back from a class C to a class B drug. A purported reason was the appearance of high potency cannabis. They believe skunk accounts for between 70 and 80% of samples seized by police[164] (despite the fact that skunk can sometimes be incorrectly mistaken for all types of herbal cannabis).[165][166] Extracts such as hashish and hash oil typically contain more THC than high potency cannabis infructescences.[167]
Laced cannabis
Hemp buds (or low-potency cannabis buds) laced with synthetic cannabinoids started to be sold as cannabis street drug in 2020.[168][169][170][171]